Genetic testing process: From blood sample to digitized DNA
Feb. 13, 2019
This paid piece is sponsored by Sanford Health.
Just as a simple blood draw gives doctors all sorts of information about our well-being, a genetic testing process called the Sanford Chip can reveal other additional information from that sample. The $49 procedure shows what medications may work better for us than others and in what doses. The test also can show whether we’re prone to some cancers or other diseases.
The Sanford Chip isn’t inserted. It’s called that because the final part of a complex process effectively bakes the person’s deoxyribonucleic acid, or DNA, onto a panel that looks like a computer chip. Sanford Health started offering the procedure in 2018 and has since completed more than 2,000 tests.
If you’re one of those people or are still researching it before deciding, here’s an explanation of the genetic testing process, simplified:
Pre-testing
This prepares the blood samples for the actual DNA testing:
- The genetic testing process starts when couriers bring blood samples from Sanford Health locations to the Sanford Imagenetics lab in coolers packed with ice, said Erika Arens, one of the genetic laboratory technicians.
- She and other lab techs unpack the samples and input the patient information into Sanford Health’s secure electronic records system to ensure that each blood sample is associated with the right person.
- The first stop for the blood sample is a robot that adds chemicals to extract DNA from the blood.
- Another machine then uses dye to quantify the DNA to determine how much of it is in the blood sample, which is different for every person.
- Next stop is a robot that normalizes, or dilutes, the samples with water to make sure they all have the same concentration of DNA — 60 nanograms per microliter. “We’re diluting the DNA (with de-ionized water) so every sample is the same concentration, so it’s easier for our robot to read everything,” Arens said.
- The last step in the initial process involves another robot attaching DNA to a plate that readies it for testing, a process called plating.
Genetic testing process
At this point, the DNA sample goes to one of two types of actual testing: pharmacogenetic or disease, which vary slightly:
Pharmacogenetic
- This begins with a robot preparing plates coated with chemicals to help determine how a person’s genetics affect how they would interact with certain prescription drugs, said Alexandra Mohror, a clinical genetics laboratory technician.
- Another robot puts the chemicals on the left side of a tray and the samples of DNA on the right side of the tray.
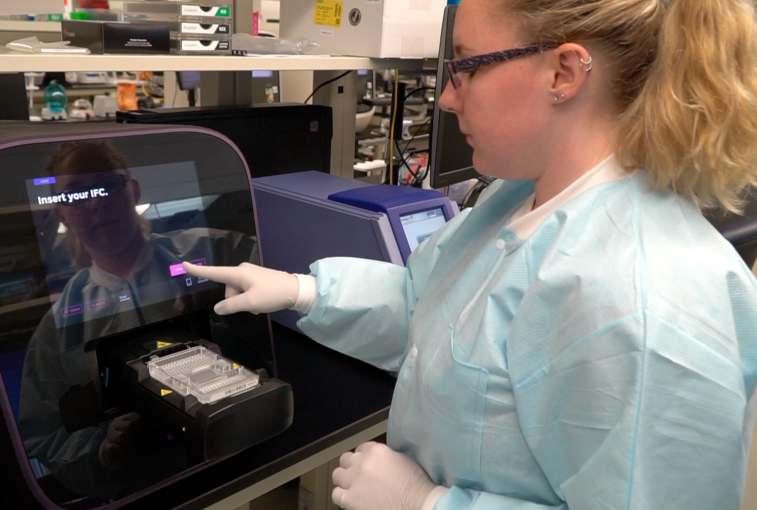
- The next step in the genetic testing process involves mixing the chemicals with the DNA, which is done by a machine called a loader. It pressurizes the plate and squeezes both sides into a gray area in the center that contains small wells where certain reactions take place.
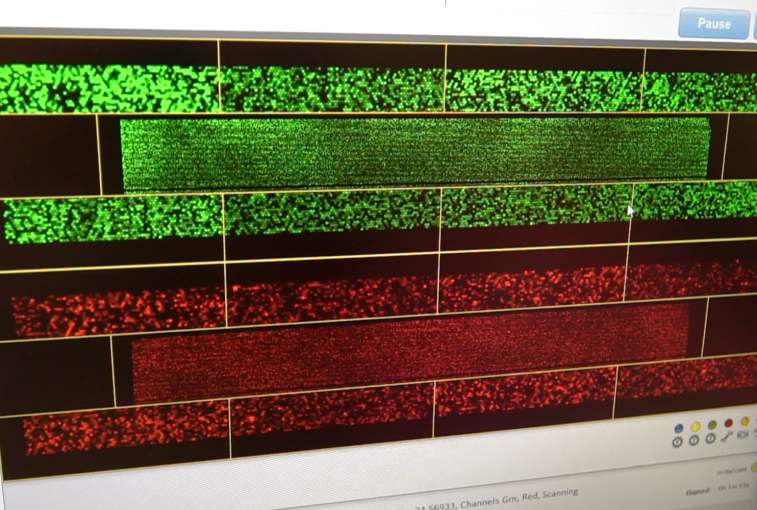
- Those reactions show up using a fluorescent dye that looks for specific parts of a person’s DNA — the actual pharmacogenetics test. This process is done through an imaging machine called the BioMark.
- The last step in the lab involves clinical genetic specialist Danny Lee reviewing everything for accuracy and determining which drugs work best for the person. The end result is more accurate prescriptions and less guessing. “By testing the patient’s DNA, it determines what kind of protein the patient will generate. And based on that protein, that’s how they metabolize a certain drug,” he said. “If a drug is simply not working based on their genetic makeup, they can switch to a different drug or they can just alter the dose to better fit the patient.”
- Finally, a lab director and pharmacist look at how the patient will break down a certain medication and use it in the body. That includes looking at the patient’s medical chart, disease management program and other things that might be going on with the person, said April Schultz, one of the pharmacists. “Then, we can take a peek at their genetics and see how that genetic profile might be affecting their medications, such as increased side effects or maybe taking one for some time without a benefit,” she said. Based on all of that, she might recommend changing the patient’s medication or dose. “We’re working to get the right drug at the right dose at the right time for the right patient.”
- The results are mailed to the patient and delivered to his or her primary physician in MySanfordChart.
Disease
- When a plate of DNA arrives for disease testing, a lab technician first adds chemicals, or reagents, to it that make millions of identical copies of the DNA for testing, said Lindsay Fricke, lead genetic laboratory specialist at the genomics lab. The samples then incubate overnight.
- The next day, a lab technician adds more chemicals to the DNA, which cuts them into smaller pieces.
- A centrifuge spins the solution to move the DNA to the bottom of the plate.
- Next, other machines add more chemicals, heat the DNA and resuspend it. That machine shakes the samples, like a paint shaker at a hardware store.
- Another robot hybridizes, or applies, the DNA to the actual Sanford Chip. There are samples from 23 people on each chip plus a control that ensures accurate results, Fricke said.
- After incubating overnight, another robot stains the chips with fluorescent dyes, which allows a scanner to read those dyes and create data used to determine the patient’s genotype, or genetic makeup.
- Lab staff and directors then use that information to determine whether that person is susceptible to certain diseases.
- The results are mailed to the patient and go into MySanfordChart.
Accuracy and privacy
After a patient’s blood sample is turned into a digital record through the genetic testing process, the focus shifts to using the information gleaned from the test to help improve his or her health.
Once lab directors verify the credibility and confirm any findings through more testing, the DNA is stored in a secure area and the information from it also is stored securely on the Sanford Chip and in the person’s electronic medical record that only the patient and his or her doctors can see. “It’s all data in your record,” Michael Mboob, director of operations for the genomics and genetics lab.
The Sanford Chip comes with the same strict privacy rules and protections as all other aspects of a person’s health care. Sanford Health stores everyone’s DNA information in a secure area, and only patients and their care providers have access to their genetic test results.
Why robots are used
Labs all over the U.S. use the Tecan robots like those used by the Sanford Chip process, Arens said. “We have some unique and more complicated applications for the robots with the normalization and plating scripts that we use. The robots bring a lot of accuracy to the process. You’re not worried about technicians accidentally pipetting (transferring liquid) into the wrong well or maybe swapping samples. They are very consistent. They will give you the same thing every time.”
Robots also speed mundane tasks.
“It does the things that would take us days or weeks to do in a matter of a few hours or a few days. They speed up the process and reduce the error rate significantly,” Mboob said.
Each instrument is named after a cartoon character, including Woody from “Toy Story” and Timon from “Lion King,” so it’s easier to identify them.
Humans are still in charge
While robots and software bring accuracy and efficiency to the process, they can do only so much and do only what they’re programmed to do, Lee said. “There’s some variability and some weirdness that the software can’t interpret, so you have to review everything to make sure the software is calling everything correctly.”
Once the Sanford Chip is run, it falls on a laboratory director like Dr. to extract meaningful information from the data generated through the genetic testing process.
That information has to be “accurate, scientifically proven and supported by evidence,” she said. “I have to put this in a format that enables the care providers, whether a primary care physician or a specialist, to use that genetic information to guide the patient care.”
Meticulous record keeping
Lab workers track and document every step and detail of the genetic testing process, including the equipment used, lot numbers of the chemicals and temperatures of the equipment and room, Fricke said. The result ensures that every aspect of the process stays within the allowable range and adds to the credibility of the lab.
“Just to run one simple test is probably 30 pages of documentation we have to follow step by step to ensure we get accurate results to the patient, and we follow the steps that are governed not only by our lab directors but also federal and state statutes as well,” Mboob said.
“I think they (patients) can take confidence in what they’re getting in terms of results is accurate, and they can rest assured it’s a quality product.”
Satisfying health care work
Just as the genetic testing process is changing health care for patients, it’s also creating new demand for people with science backgrounds needed for working in labs and research.
“I just think it’s really interesting to go from a blood sample to having results,” Arens said of her work in the lab. “I enjoy hands-on science where you start a process, you complete the process and you get results that day, as opposed to three-year-long research projects that are very specific to one thing. This is very general, and it’s got a lot of information that can help a lot of people.”